Effective infection prevention and control is essential for the delivery of quality, safe physiotherapy services. Physiotherapists must be knowledgeable about the principles underlying infection control and implement appropriate measures in their practice. This resource provides practical information to assist physiotherapists in their efforts.
Infection Prevention Control PDFEffective Infection Prevention and Control (IPC) is characterized by evidence-based practices and procedures that, when applied consistently in health-care settings, can prevent or reduce the risk of transmission of microorganisms (viruses, bacteria), also known as infectious agents. Controlling the transmission of infectious agents is essential and involves application of measures based on:
- The infectious agent in question
- How that infectious agent is transmitted and the setting
- Patient population in which the infectious agent is circulating
Physiotherapists must recognize that no single action alone will prevent the spread of infectious agents within the practice environment. It can be easy to focus on personal measures and actions that individuals can take to limit the spread of an infectious agent, as was learned early in the COVID-19 pandemic. However, it is the full complement of measures consistently applied within the practice setting which effectively limit the spread of infectious agents, render the patient, practice setting and physiotherapist safe, and can affect the health and safety of the broader community.
As the COVID-19 pandemic reinforced, effective IPC is essential for the delivery of quality, safe physiotherapy services. The COVID-19 pandemic caused physiotherapists to refine their knowledge and use of IPC measures in practice. IPC is bigger than any single virus; however, the lessons learned from the COVID-19 pandemic can help to inform and refine efforts to address the risks posed by infectious agents in practice more generally.
In accordance with the Standards of Practice and legislation governing practice, physiotherapists must maintain awareness of, and apply current, appropriate, and generally accepted infection control measures and employer-specific policies and procedures. This includes maintaining awareness of how IPC knowledge and best practices evolve over time.
Physiotherapists are expected to act with thoughtfulness towards patients and to “do what is good with respect to the welfare of their clients.” Fundamentally, physiotherapists comply with infection prevention and control best practices when providing physiotherapy services to prevent patient harm.
To achieve this outcome, physiotherapists are expected to:
- Know the IPC principles and best practices relevant to their setting and patient population
- Obtain the training necessary to apply IPC practices safely, consistently, and effectively
- Apply appropriate IPC practices consistently and effectively
The College of Physiotherapists of Alberta developed this guide to elaborate on the IPC expectations identified in the College of Physiotherapists of Alberta’s Standards of Practice and Code of Ethical Conduct and to provide practical information to help physiotherapists meet these expectations.
- Physiotherapists follow the directions and recommendations provided by public health officials and infection prevention and control professionals, especially during high levels of community transmission of infectious agents.
- Physiotherapists comply with the directions of their employers in addition to those of public health officials, recognizing that employers have a legislated responsibility to provide a safe environment for patrons and staff. This includes requiring the use of administrative, technical, and physical controls to prevent the spread of infectious agents in the workplace.
- Appropriate personal protective equipment (PPE) must be used for the safe delivery of in-person physiotherapy services, in accordance with the physiotherapist’s point-of-care risk assessment.
- Physiotherapists have a duty of care towards their patients which encompasses both the provision of safe, effective services and the mitigation of risk of harm, including risks posed by infectious agents.
Viruses and bacteria, referred to more generally as infectious agents, are ever present in the environment and are constantly adapting.2 The combination of exposure and constant mutation can lead to the emergence of:
- Novel infectious agents
- The transmission of infectious agents between animals and people3
- Emergence of drug-resistant infectious agents4
- More transmissible strains of previously known infectious agents
Each infectious agent has its own characteristics, which affect the ease with which it is transmitted (transmissibility), its ability to cause disease (pathogenicity) and the severity of illness resulting from the infectious agent (virulence).1
An infectious agent requires a reservoir or place to live. Humans, animals and the environment are all reservoirs for infectious agents. For an infectious agent to spread, it needs a way for the agent to leave the reservoir or a portal of exit. Examples include respiratory secretions (sputum), blood, and other body fluids.1
Modes of transmission include contact, droplet, airborne, vehicle (inanimate objects), and vector borne (insects or mosquitoes).1 As was learned during the COVID-19 pandemic, infectious agents:
- Can be transmitted by more than one route
- Can have different transmission characteristics under specific conditions (e.g., aerosol generating medical procedures)
- Can be transmitted by both symptomatic and asymptomatic individuals5
In some instances, an infectious agent’s transmission characteristics can change as the agent mutates.6 An example of this is the changing transmission behaviour of different variants of COVID-19.
While categorizing infectious agents as contact, droplet, airborne, vehicle, or vector borne can help to identify the measures needed to disrupt transmission and facilitate communication regarding infectious agents and how they spread, it is important to remember that “the transmission of the many varieties of microorganisms and infections they may cause cannot always be precisely circumscribed within a limited number of carefully contained transmission modes.”1 In other words, the categorization of infectious agents into these discrete categories may be an oversimplification.
Once transmitted, an infectious agent requires a portal of entry, or route by which the agent enters a new host. Finally, for an infection to occur, the individual exposed to the infectious agent must be susceptible to it.1,7
IPC measures prevent the spread of infectious agents by disrupting the chain of infection. IPC measures can target any link in the chain of infection. It is not uncommon for individuals to focus on the personal measures they can adopt to disrupt the transmission of infectious agents, such as hand hygiene and the use of personal protective equipment (PPE). However, measures such as environmental cleaning and immunization also serve to disrupt the chain of transmission.
It is essential to recognize that:
- If any link in the chain of transmission is disrupted, the spread of the infectious agent can be prevented
- There are several levels or types of measures, existing on a gradient ranging from personal to universal in their application, which can be effective at disrupting transmission
IPC measures to control or eliminate the spread of infectious agents are categorized as administrative, environmental, engineered, and personal, and are put into practice in accordance with the nature of the infectious agent and its mode of transmission.1
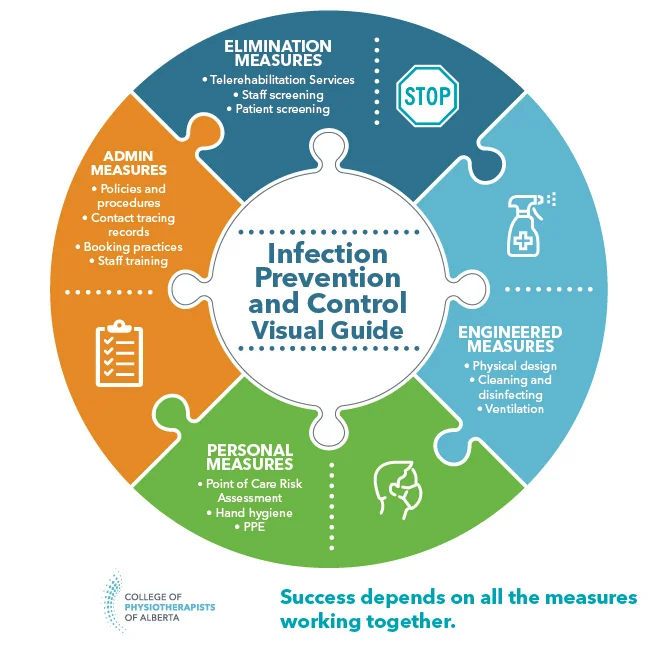

Administrative measures to control infectious agents include policies, procedures, and training used to act at a group, workplace, or community level to disrupt transmission of infectious agents. Examples include workplace sick time policies, isolation or quarantine requirements for individuals demonstrating signs and symptoms of illness, and legislation such as the Occupational Health and Safety Act (OHS Act) and the Public Health Act, which was the foundation for the provincial health orders issued during the COVID-19 pandemic.
In accordance with the OHS Act, employers are required to work with employees to identify hazards in the workplace, inform employees about hazards in the workplace, and identify appropriate controls to the hazards identified and train employees on how to mitigate the risks posed by hazards if they cannot be eliminated from the workplace. Workers (including employees and contractors) also have obligations under the OHS Act that include contributing to the identification of workplace hazards and adhering to the measures put in place by employers to address identified hazards. Infectious agents are one group of hazards that are subject to the OHS Act and the requirements for employer and worker actions.8
Additional examples of administrative measures related to IPC include:
Workplace policies:
- Regular workplace inspections and OHS committee meetings
- Workplace attendance and staff illness policies
- Patient cancellation policies and related fees when patients report they are ill
- Job descriptions specifying staff roles and responsibilities for IPC management
- Organization level PPE policies/mask requirements
Workplace training related to:
- Cleaning and disinfection practices and procedures, product use and staff responsibilities
- WHMIS training (if applicable)
- Donning, doffing and use of PPE
Government policies:
- Quarantine and isolation requirements for specific communicable diseases
- Mask mandates
- Illness reporting requirements for specific communicable diseases
While administrative measures work at a group, organization or community level, they rely on individual compliance in order to be effective to break the chain of infection.

As the name suggests, these are measures that seek to block an infectious agent from entering the practice setting. In some cases, this group of measures seek to replace hazardous work with less hazardous work. These types of controls typically change how work is designed to remove a workplace hazard, rather than relying on adherence to policies or personal measures.
Examples of elimination measures include:
- Staff and patient screening as well as access restrictions for those demonstrating signs and symptoms of illness
- Use of safety engineered sharps to reduce the risk of a needle-stick injury
- Use of virtual physiotherapy service delivery instead of in-person services when individuals demonstrate signs or symptoms of illness

These measures involve changes to the physical environment to eliminate reservoirs of infectious agents, reduce the source of the hazard, or limit the risk of exposure to the hazard.
Engineered measures differ from elimination measures as engineered measures presume that the hazard is present in the practice setting, while elimination measures seek to block the hazard from entering the practice setting.
Engineered measures can relate to:
- The design of the physical space
- Cleaning and disinfection policies and practices
The intentional design or redesign of a physical space can be used to reduce the risk of exposure to an infectious agent. These measures will be dependent on the nature of the infectious agent and how it is transmitted.
Physical design measures may include:
- Installing sharps containers and hand hygiene stations within treatment rooms or cubicles
- Selecting flooring that can be easily cleaned and disinfected
- Removing furniture that is torn, patched, or has porous surfaces
- Removing items that can not easily be cleaned and disinfected such as toys or magazines in waiting rooms
- Designating treatment cubicles and workstations for use by a single staff member
- Maintaining two to three meters of physical distancing between treatment beds, exercise equipment, workstations and seating in waiting rooms
- Installing plexiglass or other barriers to divide staff and patients at reception areas
- Prescribing traffic flow within practice settings
- Increasing ventilation by increasing air exchanges, installing air filters or opening windows
- Cohorting patients demonstrating signs and symptoms of an illness (e.g., within acute or continuing care environments)
In the context of the COVID-19 pandemic, there was considerable focus on physical distancing, space design and traffic flow within practice settings to reduce the risk of transmission of the virus. While some of these measures were not commonly used prior to the pandemic, the data related to influenza illness and death in the 2020-2021 flu season suggests that these measures may also serve to disrupt the transmission of other infectious agents.
Physiotherapists should consider which of these measures are appropriate for use on an ongoing basis within the context of their practice.
Contact is the most frequent mode of transmission of health-care associated infections and can be categorized as direct or indirect. Direct contact means physical transfer of an infectious agent from one person to another through touch. Indirect contact involves contact between a person and a contaminated object or environment.9,10
Many infectious agents, including clostridium difficile (C-diff), E. coli, influenza, norovirus, and coronavirus, are known to survive on hard surfaces with survival times ranging from hours to days or months.10 Microorganisms that can survive on inanimate surfaces can be spread by contact with contaminated surfaces which serve as reservoirs of infectious agents.
Physiotherapists can break the chain of transmission by eliminating reservoirs of infectious agents on surfaces through environmental cleaning. Effective environmental cleaning requires both cleaning and disinfection of surfaces. Cleaning refers to the removal of visible dirt and debris.11,12 Disinfection inactivates disease producing infectious agents.11 Practice settings must establish effective cleaning and disinfection practices for the surfaces and equipment used within the setting. Effective cleaning and disinfection of equipment depends on the nature of the device and its intended use.
All medical devices and equipment are categorized as either reusable, single-patient use, or single-use based on their intended use and the potential risk of infection caused by their use.11 In physiotherapy practice some devices may be used repeatedly and by several patients (e.g., gym equipment), while others may only ever be used once (e.g., solid filament needles).
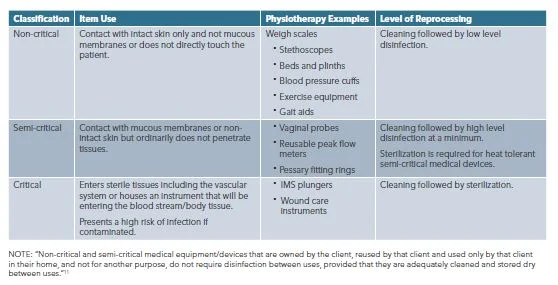
Single-patient-use and reusable medical devices are further categorized as non-critical, semi-critical, or critical, depending on whether the device is in contact with intact skin only, in contact with mucous membranes or non-intact skin, or entering sterile tissues (e.g., the vascular system).11,12
- Reusable medical equipment/devices must only be reused following appropriate reprocessing, including disinfection or sterilization.11
- Single-patient-use equipment must only be used by one patient. These devices may be reused on the same patient but may not be used on others.11
- Single use/disposable equipment must be discarded after one use. This equipment must not be reprocessed.11
See Appendix B for additional information regarding reprocessing (cleaning and disinfection) of critical and semi-critical medical devices.
Reusable, non-critical devices and equipment in physiotherapy practice include weigh scales, exercise equipment, gait aids, treatment beds, stethoscopes, and blood pressure cuffs. Other items within the practice setting may be considered “high touch” (e.g., doorknobs, pin pads used for processing payment, washroom sinks/faucets).
The frequency of routine cleaning and disinfection is dependent on the categorization and nature of the surface or item in question.
Non-critical, reusable patient care items must be cleaned and disinfected between each patient/use.12
Examples include but are not limited to:
- Treatment beds
- Exercise equipment
- Goniometers and reflex hammers
High-touch items must be cleaned and disinfected daily and more frequently as use and circumstances warrant (e.g., local disease outbreaks, level of community transmission of infectious agents).
Examples of high-touch items include but are not limited to:
- Pin pads used to process payment
- Doorknobs and light switches
- Hydrocollator handles
- Washrooms, sinks/faucets and hand sanitizer dispensers
- Counter tops, staff room desktops, clipboards, pens and shared computer keyboard/mouse
- Telephones and mobile devices
Surfaces in the practice environment that are not considered “high touch” can still be a potential reservoir for infectious agents. Cleaning and disinfection of these surfaces should occur regularly, in accordance with their use and likelihood of contamination. Examples include but are not limited to:
- Legs and undersides of treatment beds
- Cubicle curtains
- Flooring
Items that cannot be effectively cleaned and disinfected should be removed from the practice environment.13 Examples include but are not limited to:
- Magazines or toys in waiting areas
- Some exercise equipment (e.g., TheraBand)
- Chairs and other items with porous fabric upholstery
- Treatment beds or other equipment with torn or patched surfaces
Physiotherapists are expected to confirm that practice settings:
- Clean and disinfect all non-critical reusable equipment between patients, according to manufacturer’s directions
- Allocate sufficient time, staff resources and supplies to enable cleaning and disinfection, including PPE for use during cleaning and disinfection according to product requirements
- Establish clear responsibilities and accountabilities for staff involved in cleaning and disinfection activities
- Provide appropriate training for cleaning and disinfection
- Reinforce and recognize the importance of this work
All high-touch surfaces must be cleaned and disinfected when visibly soiled.
- Cleaning and disinfection are to be undertaken in accordance with manufacturer’s instructions for the equipment or device.
- Cleaning and disinfection of non-critical reusable devices and equipment should employ a “wipe twice” approach – first cleaning and subsequently disinfecting surfaces.14,15
- Virucidal disinfectants or diluted bleach solution must be used to complete the disinfection step of cleaning and disinfecting surfaces.13,16
- If using bleach, physiotherapists must follow label directions for proper dilution ratios.
- Virucidal disinfectants must have a DIN number. Physiotherapists must check the Health Canada database to confirm that the virucide in use is effective against infectious agents such as COVID-19 and other microorganisms commonly found in health-care settings.17
- Cleaning and disinfecting products must be used according to manufacturer’s directions for application and contact time.
Cleaning products that do not have a DIN or are not bleach (e.g., vinegar, tea tree oil) must not be used in clinical practice as they are not proven effective and are not approved for use.
WHMIS18 is a system that provides workers with information about hazardous products in the workplace. The system consists of:
- Hazard classifications
- Mandatory labelling on hazardous products that provides information about the product and precautions to be taken when in use
- Safety data sheets
- Education and training programs
The system is designed to ensure that all employers and workers receive consistent reporting related to the chemical hazards they may encounter in the practice setting and are properly trained about the use of hazardous materials.
WHMIS is relevant to the discussion of IPC because the chemicals used for cleaning and disinfection and the reprocessing of reusable medical devices can pose a hazard to employees who perform cleaning, disinfection, and reprocessing. These chemicals may be subject to the rules and related requirements of the WHMIS system and when used in the physiotherapy practice environment, physiotherapists and employers must fulfill the legislated requirements of WHMIS.
However, the chemicals used in a practice setting for cleaning and disinfection may also be classified as consumer products. Consumer products are those products that can be purchased in a store and are generally intended to be used in the home. Consumer products are not covered by WHMIS.
While cleaning and disinfecting products may or may not be subject to WHMIS requirements, employers have a legislated responsibility according to OHS law to:
- Inform employees about hazards in the workplace
- Provide controls to mitigate the risks posed by hazards
- Train employees in the safe use of both products and controls8
In all instances physiotherapists are advised to follow manufacturer’s instructions regarding the safe use and storage of the chemicals they use within the practice setting.

Personal measures consist of actions that individual physiotherapists, acting independently, can take to reduce the risk of spread of infectious agents and their personal risk of becoming ill. Personal measures include:
- Point of Care Risk Assessment
- Hand hygiene
- Person Protective Equipment (PPE) Use
- Immunization
As already stated, OHS legislative requirements include the employer requirement to provide information and training about hazards present in the practice environment. This includes requirements to provide and train staff in the use of PPE. Worker duties under OHS legislation which include identifying risks and hazards in the practice environment, and making employers aware of these hazards and working collaboratively to mitigate hazards, include employing the PPE and other measures in place to mitigate identified hazards.8
Point of care risk assessments19,20 are a mainstay of safe clinical practice. Point of care risk assessments involve the identification of all relevant risks before engaging in a patient interaction and may encompass risks related to:
- Patient factors (e.g., patient cognition, patient agitation)
- Environmental risks (e.g., slip, trip and fall hazards)
- Practice setting risks (e.g., work in isolation)
- The likelihood of exposure to infectious agents
A point of care risk assessment is based on the physiotherapist’s professional judgment about the clinical situation and assists the physiotherapist to take appropriate actions and make decisions to minimize identified risks.
Specific to point of care risk assessment and infectious agents, physiotherapists must:
A. Be well informed about:
- Infectious agents relevant to the physiotherapy services they offer, their practice location, and local infectious disease trends
- The transmission characteristics of relevant infectious agents
- The measures appropriate to mitigate the risk of spread of those agents
B. Complete a point of care risk assessment prior to every patient interaction, assessing:
- The task (What assessment or treatment procedures are planned or conducted?)
- The patient (Health status, willingness and ability to perform hand hygiene or respiratory hygiene, and wear PPE if appropriate)
- The environment
- Health and immunization status of people in practice environment including the physiotherapist, colleagues and other patients
- Degree of infection risk present in the practice setting and community at large (including local, national and international considerations as appropriate)
C. Based on this assessment, determine the risk of exposure to blood or body fluids and infectious agents and the PPE required to mitigate the risk and perform the patient care task safely
D. Consider their own risk tolerance when determining whether to provide in-person physiotherapy services and the personal protective equipment to employ
Risks exist on a continuum. There is no one-size-fits-all answer for the question of which infection control measures are needed for all clients in all practice settings and in relation to all infectious agents. This is why physiotherapists must use critical thinking and clinical judgment on a case-by-case basis to assess risk and act accordingly.
Hand hygiene is widely recognized as the single most important IPC practice; however, some estimates indicate that compliance with routine hand hygiene practices is as low as 40% among health professionals.21,22
Routine, effective hand hygiene helps to break the chain of transmission by acting on one of the primary modes by which infectious agents are spread: health-care workers.
Physiotherapists are expected to practice routine hand hygiene consistent with the World Health Organization’s “5 Moments for Hand Hygiene:”22
- Before touching a patient
- Before clean/aseptic procedures
- After body fluid exposure or risk
- After touching a patient
- After touching patient surroundings
Hand hygiene can be completed using alcohol-based hand rub or hand washing using soap and water.
- Alcohol-based hand rub must have a minimum alcohol content of 60% to be effective24
- When hands are visibly soiled, they must be cleaned with soap and water24
Hand hygiene practices should also consider practice setting and the disease-specific recommendations that apply to some infectious agents (e.g., soap and water is the recommended method for hand hygiene after working with patients with C-difficile).1,23
Hand hygiene facilities should also be available to patients, and patients should be encouraged to complete hand hygiene using soap and water or alcohol-based hand rub:
- Upon arrival at the practice setting
- Before and after use of shared equipment such as weights or other exercise equipment
- Prior to processing payment
- Prior to departure from the practice
Other basic hygiene considerations include:
- Avoiding touching one’s face
- Practicing respiratory etiquette by coughing or sneezing into one’s elbow or covering coughs and sneezes with a facial tissue and disposing of the tissue immediately25
PPE may be the first thing that comes to mind when thinking of IPC measures, as the use of PPE is in the individual physiotherapist’s control. However, these measures are considered the weakest IPC measures because they require consistent individual adherence to be effective.1
Physiotherapists routinely use gloves, gowns and masks as barriers between themselves and contagious infectious agents. Other examples of PPE include goggles and face shields. During the COVID-19 pandemic, all physiotherapists had cause to review the indications for different PPE and the correct way to don and doff PPE.
PPE use by physiotherapists should be:
- One part of a comprehensive collection of measures employed in the practice setting to mitigate the risks posed by infectious agents present and tasks performed
- Implemented based on the findings of the Point of Care Risk Assessment
- Supported by education and training related to:
- Infectious agents present in the practice environment
- The PPE indicated to address those agents*
- Procedures for the correct implementation, donning and doffing of PPE
*In public practice settings, IPC professionals will typically provide direction regarding the PPE indicated for a patient’s symptoms or known infection. Additional information regarding PPE selection for different infectious agents is available through Alberta Health Services.26
The College of Physiotherapists of Alberta supports immunization as “one of the world’s greatest public health achievements.”27 Immunization saves lives and reduces the chances of debilitating long-term illness. “For over 50 years, vaccines have helped prevent and control the spread of deadly diseases and saved the lives of millions of infants, children and adults.”27 Vaccines are rigorously researched and tested, and are evaluated for their safety, efficacy, and quality prior to being authorized for use by Health Canada.
Immunization protects the health and wellbeing of physiotherapists and other health-care workers who are vital to the health system.
Research has indicated that health-care workers are considerably more likely to contract the flu or to be asymptomatic carriers of the flu virus than members of the public.28 Historically, health-care workers have also been known to attend work despite being mildly ill and, therefore, pose a risk of transmission to others.28
Physiotherapists routinely work with individuals who are very ill and are often in close contact with their patients. The risk of a susceptible patient coming into close contact with a physiotherapist who is pre-symptomatic or mildly symptomatic with an infectious disease is greater than the risks posed by general interpersonal interactions or interactions between non-health care professionals and their clients.
Immunization, when not medically contraindicated, is one measure physiotherapists can adopt to support the health and safety of clients, themselves, and others, and is aligned with the expectations articulated in the Standards of Practice and Code of Ethical Conduct.29,30
The College of Physiotherapists of Alberta strongly encourages all physiotherapists to be vaccinated against infectious agents present in their communities and practice environments, including COVID-19, for the protection and safety of patients, colleagues and themselves.
As trusted health professionals, physiotherapists can also play a role in supporting public health initiatives such as mass immunization programs. Physiotherapists can do so through role modelling and by amplifying credible messages and information regarding vaccine development, efficacy and safety to their peers and patients. Physiotherapists are encouraged to seek information from credible sources to inform themselves of the vaccines approved for use in Canada, the approval process, and the risk profiles of vaccines.
Physiotherapists are directed to Health Canada’s website for additional information about the vaccine approval process.
The information in this appendix provides direction for responding to periods of high transmission of infectious agents, such as local outbreaks or epidemics of respiratory illnesses, including potential future waves of the COVID-19 pandemic. Respiratory illness outbreaks include outbreaks of COVID-19, influenza, or other infectious agents known to spread via respiratory droplets or aerosols.
This information:
- Is intended to supplement and should be reviewed in conjunction with the general information contained in this guide
- Outlines recommended physiotherapist actions during periods of high transmission of infectious agents that cause respiratory illness
- Should be reviewed alongside any specific directions or public health orders issued by Alberta Health or the Chief Medical Officer of Health
In instances where the recommendations of Alberta Health or the Chief Medical Officer of Health differ from that of the College, physiotherapists are to adhere to the directions of Alberta Health and the Chief Medical Officer of Health.
When high levels of community transmission of an infectious agent are occurring:
- Physiotherapists will seek credible information and resources regarding the infectious agent and how it is transmitted
- In-person services must only proceed when the anticipated benefits outweigh the risks posed to the patient and the physiotherapist by those services
- The physiotherapist is accountable and is the person best positioned to determine the need for, urgency and appropriateness of in-person services
- Services that can be provided safely and effectively via virtual physiotherapy, should be
During respiratory illness outbreaks, physiotherapists review organization policies and procedures, and any training or education requirements (including re-training) to address the risks related to the infectious agent.
Relevant policies and procedures to review, modify or implement may include but are not limited to:
- Patient screening for signs and symptoms of illness prior to attending the practice setting
- Cancellation policies and fees, and attendance/rebooking practices for patients reporting illness
- The number of individuals admitted to the practice setting at a given time, (e.g., staggering appointment times and limiting time in waiting areas)
- Targeted actions to address specific patient subgroups (e.g., designating booking blocks for individuals at higher risk of severe outcomes)
- Maintaining attendance records for the purpose of contact tracing
- Staff screening for signs and symptoms prior to attending work, as well as staff attendance policies and sick time allocations
- Roles and expectations for cleaning and disinfection of equipment and surfaces
Physiotherapists and their employers are advised to:
- Collaborate to develop policies and procedures to screen patients upon arrival at the practice setting
- Recognize that some patients may not be forthcoming in reporting respiratory symptoms
- Develop a common script to use when discussing organizational policies with patients
- Provide clear guidance for when to decline or discontinue treatment for symptomatic patients
- Consider how policies related to sick time and work attendance or appointment cancellation may incentivise attendance when ill and whether such policies should be suspended during illness outbreaks or epidemics or discontinued entirely
Training should include, but is not limited to:
- A review of the basics of infection prevention and control
- Fundamentals of disease transmission
- Specific information related to the infectious agent outbreak, the agent’s transmission, and signs and symptoms of illness
- Controls to limit the risk of transmission
- The correct application and use of personal protective equipment
It is recommended that physiotherapists and other workers in the practice setting review this information again in the context of new respiratory illness outbreaks or successive waves of COVID-19.
There are some settings in which elimination measures may not be appropriate (e.g., acute care environments, where patients may seek care for acute illness related to the infectious agent). In community settings, elimination may be an appropriate objective.
Patient Screening
Physiotherapists working in community settings should engage in active screening of patients when patients are seeking physiotherapy services for conditions not related to the outbreak, epidemic or pandemic. Physiotherapists are advised to screen patients for:
- Signs and symptoms of illness when booking appointments and upon patient arrival
- Recent close contact with individuals who have been diagnosed with the illness in question, or who are displaying signs and symptoms of illness
- Known risk factors for illness (e.g., travel)
- The presence of isolation, quarantine or other requirements established by public health officials
Physiotherapists should use the screening process to inform the point of care risk assessment, first determining the appropriateness of in-person services and subsequently the need for additional measures to mitigate the risk of spread of the infectious agent in the practice setting.
Physiotherapists may choose to defer in person services for individuals with signs and symptoms of illness, consistent with infection prevention and control best practices.
Virtual physiotherapy
Physiotherapists should also continue to employ virtual physiotherapy when practicable to achieve desired patient outcomes. When employing virtual physiotherapy service delivery physiotherapists are encouraged to:
- Educate patients on the benefits and limitations of virtual physiotherapy services
- Consider virtual physiotherapy as the sole means of service delivery when practicable and indicated by the patient’s condition and/or the risk assessment
- Adopt blended models of service delivery (using both virtual physiotherapy and in-person care) as appropriate
- Recognize when physiotherapy assessments or treatments cannot reasonably be delivered via virtual physiotherapy
Self-Screening
Physiotherapists are also advised to engage in self-screening, closely monitoring for signs and symptoms of illness and their own history of contact with people who are ill.
When public health directives related to isolation or quarantine are in effect, physiotherapists must comply with these directives.
In the absence of directives from public health officials to quarantine or isolate when ill, physiotherapists who develop signs and symptoms of illness are advised to reflect on their duties to patients and others as established by the Standards of Practice, Code of Ethical Conduct, Occupational Health and Safety legislation, and employer policies when determining whether it is appropriate to attend work.
Physical Design
In the context of an outbreak, physiotherapists should review the use of measures such as:
- Physical distancing in treatment areas and waiting rooms (two meters or more depending on the activity considered)
- Use of one-way movement and direction signage
- Prevention of patient or staff congregation in areas of the practice setting
- Physical barriers (e.g., plexiglass) between patients and administrative staff
- Increased ventilation and use of air filters when appropriate
During times of high disease transmission, physiotherapists should avoid sharing equipment or treatment rooms, when feasible.
Cleaning and Disinfection
During times of high disease transmission:
- Surfaces should be cleaned and disinfected more frequently (e.g., increase frequency of cleaning and disinfection of high touch surfaces to more than once a day)
- Responsibilities for cleaning and disinfecting activities should be clearly articulated
- Physiotherapists must ensure:
- Adequate supplies and resources are dedicated to cleaning and disinfection
- That manufacturer’s directions for use of cleaning and disinfecting products (e.g., application and contact times) are followed
Masks
The College of Physiotherapists of Alberta recommends that physiotherapists engage in continuous masking when in the workplace and providing direct patient care in the context of high respiratory disease transmission.
Physiotherapists are advised to consider mask use as one component of a suite of measures they put in place to manage the risk of spreading respiratory illnesses within the practice setting. Masks:
- Should be well-fitting
- Should have appropriate filtration properties for the infectious agent considered
- Must be changed when they become wet or soiled31
Physiotherapists must be aware of public health mandates regarding mask use in public spaces or within health-care settings and must comply with legislation relevant to their practice.
Patient Use of Masks
Physiotherapists may ask patients to wear a mask during physiotherapy treatment.
IF a patient declines to wear a mask, and the physiotherapist or physiotherapy business is considering requiring mask use as a condition of service due to an outbreak or high local disease transmission, physiotherapists are reminded that:
- Physiotherapists are required to be knowledgeable of and compliant with the legislation relevant to their practice. This includes having knowledge of provincial legislation or mandates and municipal bylaws relevant to their community and practice setting
- Physiotherapists are expected to promote and maintain a safe environment for clients, health-care providers, themselves and others
- Members of the physiotherapy profession have an ethical responsibility to “Act in a respectful manner and do not refuse care or treatment to any client on the prohibited grounds of discrimination as specified in the Canadian Human Rights Act as well as on the grounds of social or health status”29
Declining to provide care is a serious matter. There are conflicting needs, values and rights involved in such a decision.
Physiotherapists and physiotherapy business owners should understand the many implications if they are considering refusing to provide care to a patient who declines to wear a mask in the practice setting.
Providing In-Person Services to Unmasked Patients
If a physiotherapist opts to provide in-person services to an individual who declines to wear a mask during an outbreak or period of high local disease transmission, the physiotherapist must consider all the measures they can put in place to render the service safe for the patient and for other patients who may be present in the practice setting, including, but not limited to:
- Use of virtual physiotherapy
- Scheduling the patient during a quiet time of day or designating booking times for high-risk patients and not booking the patient in question during these times
- Enhancing other safety measures in use in the clinic before, during, and after the patient in question attends (e.g., increasing ventilation, treatment in a private room)
- Enhanced PPE use by the physiotherapist
Eye Protection
Eye protection is used when high levels of community transmission of respiratory viruses are occurring, as an added layer of protection when interacting with patients within two meters.
Eye protection is a strategy to reduce the physiotherapist’s individual risk of becoming ill. Physiotherapists may consider using eye protection as part of their routine point of care risk assessment and PPE use.32
Examples of appropriate eye protection include safety glasses, reusable goggles, face shields or face masks with built-in eye shields.33 Vision correcting eyeglasses are not classified as eye protection and do not address PPE recommendations.
Some eye protection is single use, while other products are reusable following cleaning and disinfection. Follow manufacturer instructions regarding whether eye protection is reusable and the approved cleaning and disinfecting products and frequency for the eye protection product in use.
Other PPE
Other PPE may not be required to prevent the spread of infectious agents when working with asymptomatic patients. However, physiotherapists should assess the tasks they are planning and continue to employ PPE typically used when performing the interventions planned (e.g., gloves when needling).
Physiotherapists are advised to wear a well-fitting medical grade surgical or procedure mask or a well-fitting KN95 facemask, at all times, and in all areas of the workplace when providing direct care to patients who are asymptomatic and are not presumed, suspected, or confirmed to have COVID-19.33
PPE Use When Working with Patients with COVID-19
Physiotherapists working with patients known or suspected of having COVID-19 in ICU, acute care, or continuing care environments, are to follow their employer’s directions regarding PPE use with this patient population and for the tasks performed.
The College of Physiotherapists of Alberta recommends that physiotherapists working in community-based environments conduct a point of care risk assessment and consider their responsibilities as articulated in the Code of Ethical Conduct, Standards of Practice, and Occupational Health and Safety legislation when deciding whether to provide in-person services to individuals with known or suspected COVID-19.
PPE recommendations when working with patients with known or suspected COVID-19, including those with respiratory symptoms are:33
- A fit tested N95 or a seal-checked KN95 respirator (if a fit-tested N95 is not available or the individual has not been fit-tested)
- Protective eyewear (goggles or face shield)
- Gown and gloves as indicated by the point of care risk assessment
Hand Hygiene
Hand hygiene practices and requirements are unchanged in the context of an outbreak, epidemic or pandemic. However, compliance with routine, consistent hand hygiene has been a concern of infection prevention and control experts for many years. In the context of an outbreak, epidemic or pandemic, physiotherapists are advised to redouble their efforts to ensure their hand hygiene practices are consistent with best practices and consider actions such as hand hygiene audits to facilitate compliance.
Contact Tracing
In future outbreak situations, or future waves of the COVID pandemic, physiotherapists are advised to implement what they have learned during the COVID-19 pandemic:
- Physiotherapists may not be contacted by public health officials when they are a close contact of someone with COVID-19 or other respiratory illness.
- Physiotherapists may be contacted by patients reporting they are ill, and that the physiotherapist has been exposed to the illness.
- Physiotherapists are routinely in close contact with individuals (less than two meters away) for longer than 15 minutes (cumulative).
- Use of appropriate PPE for the patient’s presentation and rigorous hand hygiene helps to mitigate the risk of being considered a close contact if a patient becomes ill.
- Close contact status affects the risks that the physiotherapist may pose to other patients and the actions the physiotherapist may need to take to mitigate those risks.
- Specific to COVID-19, if a physiotherapist becomes symptomatic, all the patients who they cared for in the 48 hours prior to symptom onset will NOT be considered close contacts if the physiotherapist wore a well fitting surgical/procedure mask or well-fitting KN95 mask and practiced routine, frequent hand hygiene.33
All medical devices and equipment are categorized as reusable, single-patient use, or single-use based on their intended use and potential to become a route of transmission of an infectious agent.11
In physiotherapy practice some devices may be used repeatedly and by several patients (e.g., gym equipment), while others may only ever be used once (e.g., solid filament needles).
Reusable medical equipment/devices must only be reused following appropriate reprocessing, including cleaning and disinfection or sterilization.11
Single-patient-use equipment must be used by one patient only. These devices may be reused on the same patient but may not be used on others.11
Single-use/disposable equipment must be discarded after one use. This equipment must not be reprocessed.11
Medical device reprocessing refers to the process required to clean and disinfect or sterilize all reusable equipment between patients. Devices must be cleaned before they can be disinfected or sterilized. All equipment must be cleaned and disinfected or sterilized between patients.
Cleaning involves the physical removal of foreign material from equipment. Cleaning physically removes rather than kills microorganisms.12
Disinfection results in the inactivation of disease producing microorganisms, but disinfection does not destroy bacterial spores.11,12
Sterilization is a multistep process that results in the destruction of all forms of microbial life including bacteria, viruses, spores, and fungi.11,12
Manufacturer’s Directions
All medical devices and equipment approved for use in Canada are required by Health Canada to include manufacturer’s instructions for the appropriate use and reprocessing of the device or equipment.12 Manufacturer’s instructions must take into consideration the intended use and potential risk of infection arising from the use of the device.
Spaulding Classification
In addition, the Spaulding Classification divides reusable medical devices into three categories based on their intended use and the potential risk of infection involved in their use. The Spaulding Classification provides guidance on the level of reprocessing required for reusable devices belonging to each category.12
If there is a discrepancy between the reprocessing level recommended by the manufacturer and the reprocessing requirements according to the Spaulding Classification, the higher level of reprocessing must be used.11
Detailed information regarding the knowledge, skills, equipment and methods required to engage in high level disinfection or sterilization of semi-critical or critical equipment is beyond the scope of this document.
Physiotherapists are reminded that should their practice include the use of semi-critical or critical devices, or devices which according to manufacturer’s instructions require high level disinfection or sterilization, they are responsible to ensure that these devices are used and reprocessed according to manufacturer’s instructions.
Physiotherapists must carefully consider whether they have the necessary resources, skills, competence and equipment to engage in medical device reprocessing. Physiotherapist are reminded that they may hire third party contractors to engage in reprocessing on the physiotherapist’s behalf. When doing so, the physiotherapist retains ultimate responsibility to ensure that the third party has the skills, competence and equipment necessary to complete the activity effectively.
Physiotherapists must also ensure that they have the correct facilities to appropriately store used devices and equipment awaiting collection by third parties for reprocessing to prevent damage to equipment to be reprocessed, and cross contamination between equipment to be reprocessed and sterile or disinfected equipment.11
Further information regarding reprocessing of semi-critical and critical devices can be found at:
- College of Physicians and Surgeons of Alberta. Medical Device Reprocessing
- Alberta Health Services. Medical Device Reprocessing – Decentralized Medical Device Reprocessing
- Public Health Agency of Canada. Routine Practices and Additional Precautions for Preventing the Transmission of Infection in Healthcare Settings. 2013. Retrieved from: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/diseases-conditions/routine-practices-precautions-healthcare-associated-infections/routine-practices-precautions-healthcare-associated-infections-2016-FINAL-eng.pdf Accessed July 25, 2022.
- W.R. Fleischmann. Viral Genetics. In Medical Microbiology. 4th ed. Baron S ed. 1996. Galveston Tx. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK8439/ Accessed July 25, 2022.
- Woodhouse M, Scott F, Hudson Z, Howey R, Chase-Topping M. Human viruses: Discovery and Emergence. Philosophical Transactions of the Royal Society B Biological Sciences. 2012 Oct 19; 367(1604): 2864–2871. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3427559/ Accessed July 25, 2022.
- Centers for Disease Control and Prevention. How Antimicrobial Resistance Happens. 2021. Available at: https://www.cdc.gov/drugresistance/about/how-resistance-happens.html Accessed July 25, 2022.
- Government of Canada. COVID-19: Prevention and Risks. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks.html Accessed September 2, 2022.
- Centers for Disease Control and Prevention. Variants of the Virus. Available at: https://www.cdc.gov/coronavirus/2019-ncov/variants/index.html Accessed September 2, 2022.
- Infection Prevention and You. Break the Chain of Infection. Available at: https://infectionpreventionandyou.org/protect-your-patients/break-the-chain-of-infection/#:~:text=The%20six%20links%20include%3A%20the,of%20entry%2C%20and%20susceptible%20host.&text=The%20way%20to%20stop%20germs,this%20chain%20at%20any%20link Accessed July 25, 2022.
- Province of Alberta. Occupational Health and Safety Act. 2022. Available at: https://www.qp.alberta.ca/documents/Acts/O02P2.pdf Accessed July 25, 2022
- Government of Nunavut. Infection Prevention and Control Manual. Modes of Transmission. N.d. Available at: https://www.gov.nu.ca/sites/default/files/files/4_%20Modes%20of%20Transmission%20-%20march%205%20-%20low%20re Accessed July 25, 2022.
- Kramer, A., Assadian, O. (2014). Survival of Microorganisms on Inanimate Surfaces. In: Borkow, G. (eds) Use of Biocidal Surfaces for Reduction of Healthcare Acquired Infections. Springer, Cham. https://doi.org/10.1007/978-3-319-08057-4_2
- Public Health Ontario. Best Practices for Cleaning, Disinfection and Sterilization of Medical Equipment/Devices in All Health Care Settings, 3rd Edition. Available at: https://www.publichealthontario.ca/-/media/Documents/B/2013/bp-cleaning-disinfection-sterilization-hcs.pdf?sc_lang=en Accessed July 25, 2022.
- Alberta Health. Reusable & Single-Use Medical Devices Standards: Standards for the reprocessing of reusable medical devices and for the use of single-use medical devices in all health care facilities and settings. 2019. ISBN 978-1-4601-4547-0 Available at: https://open.alberta.ca/dataset/fd371ac2-b2be-49ac-93ef-43865a0bc0fb/resource/56c1cd3c-b617-4d91-947d-3e0e4a68cd09/download/health-reusable-single-use-medical-devices-standards.pdf Accessed July 25, 2022.
- Public Health Ontario. Best Practices for Environmental Cleaning for Prevention and Control of Infections in All Health Care Settings, 3rd edition. 2018. Available at: https://www.publichealthontario.ca/-/media/documents/B/2018/bp-environmental-cleaning.pdf Accessed July 25, 2022.
- Centers for Disease Control and Prevention. Cleaning and Disinfecting Environmental Surfaces. 2016. Available at: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/cleaning-disinfecting-environmental-surfaces.html Accessed July 25, 2022.
- Alberta Health Services. Key Points for Ready-to-Use (RTU) Pre-Moistened Disinfectant Wipes. 2021 Available at: https://www.albertahealthservices.ca/assets/healthinfo/ipc/if-hp-ipc-bpg-ready-to-use-wipes-info.pdf Accessed July 25, 2022
- British Columbia Centre for Disease Control. Cleaning and Disinfecting. 2022. Available at: http://www.bccdc.ca/health-info/diseases-conditions/covid-19/prevention-risks/cleaning-and-disinfecting Accessed July 25, 2022.
- Government of Canada. Hard-Surface Disinfectants and Hand Sanitizers (COVID-19): List of Disinfectants with Evidence for use Against COVID-19. Available at: https://www.canada.ca/en/health-canada/services/drugs-health-products/disinfectants/covid-19/list.html Accessed July 25, 2022.
- WorkSafeBC BC. WHMIS 2015 – At Work. Available at: https://www.worksafebc.com/en/health-safety/hazards-exposures/whmis/whmis-2015 Accessed July 25, 2022.
- College of Physical Therapists of British Columbia. Point of Care Risk Assessment. 2021. Available at: https://cptbc.org/wp-content/uploads/2021/04/POCRA_April14_2021_a.pdf Accessed July 25, 2022.
- Alberta Health Services. Point of Care Risk Assessment (PCRA). 2022. Available at: https://www.albertahealthservices.ca/assets/healthinfo/ipc/hi-ipc-acute-care-pcra.pdf. Accessed July 25, 2022.
- Erasmus, V., Daha, T., Brug, H., Richardus, J., Behrendt, M., Vos, M., & Van Beeck, E. (2010). Systematic Review of Studies on Compliance with Hand Hygiene Guidelines in Hospital Care. Infection Control & Hospital Epidemiology, 31(3), 283- 294. doi:10.1086/650451
- World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care. 2009. WHO Press. Geneva.
- Centers for Disease Control and Prevention. FAQs for Clinicians about C. Diff: How Can CDI Be Prevented in Hospitals and Other Healthcare Settings? 2022. Available at: https://www.cdc.gov/cdiff/clinicians/faq.html#:~:text=As%20no%20single%20method%20of,hand%20hygiene%20after%20removing%20gloves Accessed July 25, 2022.
- British Columbia Centre for Disease Control. Hand Hygiene. Available at: http://www.bccdc.ca/health-info/prevention-public-health/hand-hygiene Accessed July 25, 2022.
- Centers for Disease Control and Prevention. Respiratory Hygiene/Cough Etiquette in Healthcare Settings. Available at: https://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm Accessed July 25, 2022.
- Alberta Health Services. Isolation Pocket Reference for ADULTS. Available at: https://www.albertahealthservices.ca/assets/healthinfo/ipc/hi-ipc-revised7-isolation-pocket-reference-pr.pdf Accessed September 2, 2022.
- Government of Canada. Regulating Vaccines for Human Use in Canada. Available at: https://www.canada.ca/en/health-canada/services/drugs-health-products/biologics-radiopharmaceuticals-genetic-therapies/activities/fact-sheets/regulation-vaccines-human-canada.html Accessed February 1, 2021.
- Association for Professionals in Infection Control and Epidemiology. APIC Position Paper: Influenza vaccination should be a condition of employment for healthcare personnel, unless medically contraindicated. 2011. Available at: http://www.apic.org/Resource_/TinyMceFileManager/Advocacy-PDFs/APIC_Influenza_Immunization_of_HCP_12711.pdf Accessed July 25, 2022.
- College of Physiotherapists of Alberta. Code of Ethical Conduct. Available at: https://www.cpta.ab.ca/docs/197/Code_of_Ethical_Conduct.pdf Accessed July 25, 2022.
- College of Physiotherapists of Alberta. Safety Standard of Practice. Available at: https://www.cpta.ab.ca/for-physiotherapists/regulatory-expectations/standards-of-practice/safety/ Accessed July 25, 2022.
- Alberta Health Services. AHS Guidelines for Continuous Masking. Available at: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-ppe-continuous-use-guidance-masking.pdf Accessed July 25, 2022.
- Alberta Health Services. Personal Protective Equipment (PPE) Frequently Asked Questions. 2022. Available at: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-ppe-faq.pdf Accessed July 25, 2022.
- Alberta Health. Alberta Public Health Disease Management Guidelines: Coronavirus, COVID-19. July 2022. Available at: https://open.alberta.ca/dataset/a86d7a85-ce89-4e1c-9ec6-d1179674988f/resource/6616d157-5b8d-4b2e-bfec-da5ba9afca48/download/health-phdmg-coronavirus-covid-19-2022-07.pdf Accessed July 25, 2022.




